Infection From An Insulin Pump
Infection From An Insulin Pump
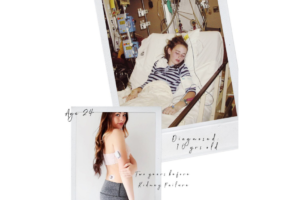
By: Brittany Gilleland
I’ve been an Omnipod pump user for over 5 years. And in that 5 years I’ve lowered my A1C and experienced a more comfortable, flexible quality of life. But this past week I’ve experienced a potentially life-threatening scenario due to the Omnipod.
Before I go into detail, I will add that this scenario can happen to anyone (diabetic or not). It just so happens when dealing with needles and puncturing our skin it leaves vulnerability for infections. I will continue on using the Omnipod because I see more of a benefit than a risk (as long as I proceed with special care). *This also happen on ANY kind of insulin pump*.
So, a week ago after a site change I noticed a small lump underneath my skin.
This bump is normal to me being that skin can become irritated. I’m used to getting insulin trapped underneath and tape causing irritation. I continued on with my day not thinking too much of it.
Then later on I noticed that it was throbbing, red, and warm to the touch.
My husband then looked at it and said it looked similar to what he had before called “cellulitis” and to keep a close eye on it.
However, it was hard to ignore, it was unlike anything I’ve experienced before. I started to become fatigued and almost like I was coming down with the flu. A big red flag for me was that my blood sugar numbers were higher than normal and very resistant. I questioned whether or not to go to the ER since it was late in the day.

I posted a status in my diabetes group and everyone said better get it checked out and play it safe.
Once getting checked into the ER and evaluated. The doctor described it as a “boil” and performed an ultrasound (which a small pocket of infection was found). So then they numbed it and lanced it. The doctor then sent me home with Bactrim (an antibiotic) and to come back if it gets worse. I thought this was odd because of my medical history and the fact that the area had gotten worse so quickly.
The following day, I felt even worse. I was running a high temperature and laid in bed all day.
I picked up my antibiotic and hoped that I would fight this infection once the antibiotic ran its course. However, the redness and swelling proceeded to engulf my arm. I took ibuprofen to subside the pain and fever and hopefully by the next day I would feel better.

By the 3rd day I decided to check myself back into the ER. First glance by the doctor, she said that she’d be admitting me. She explained, generally they give oral antibiotics first and do IV antibiotics if that fails. At this point, I was okay because the Bactrim helped eliminate the pain but it was continuing to spread along my arm.
For the next 2 days, it was a wait and see approach to see if the IV antibiotics and another irrigation could clear up the infection. The doctors were amazed by how an insulin pump was the cause of my infection.
The whole visit was really eye opening to see how little many doctors are educated about type 1 diabetes and the intensive care it involves. I took the reigns on the majority of my blood sugar and insulin management.

Soon doctors realized that the infection was still spreading and not getting better. The culture revealed that the bacteria was STAPH.
The surgeon scheduled me for surgery for an I&D (incision and drainage). I was really nervous about anesthesia as this would be the first time not being in complete control over my diabetes.
Thankfully though, the procedure went fine. The wound was packed and wrapped. The following day I was able to go home. This experience was frightening because diabetes was in the mix. Diabetes is hard enough on my body and adding in an infection, makes things 10x more complicated.

One thing I’ve learned is to ALWAYS take any potential infection serious.
And to use alcohol wipes to ensure pump/injection sites are thoroughly clean. I will definitely be taking extra precaution in the future.