Thank God I Woke Up
By: Katharine Orona
Blog: This is Type 1 Diabetes
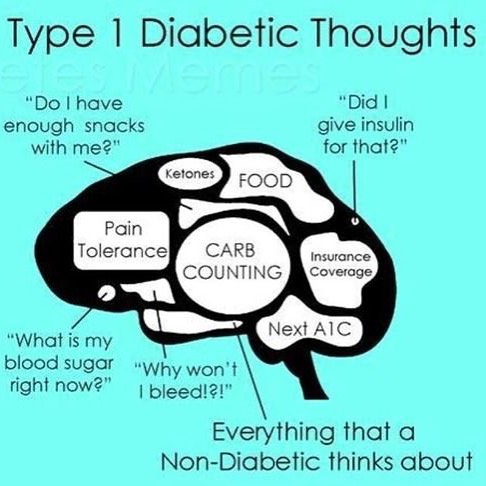
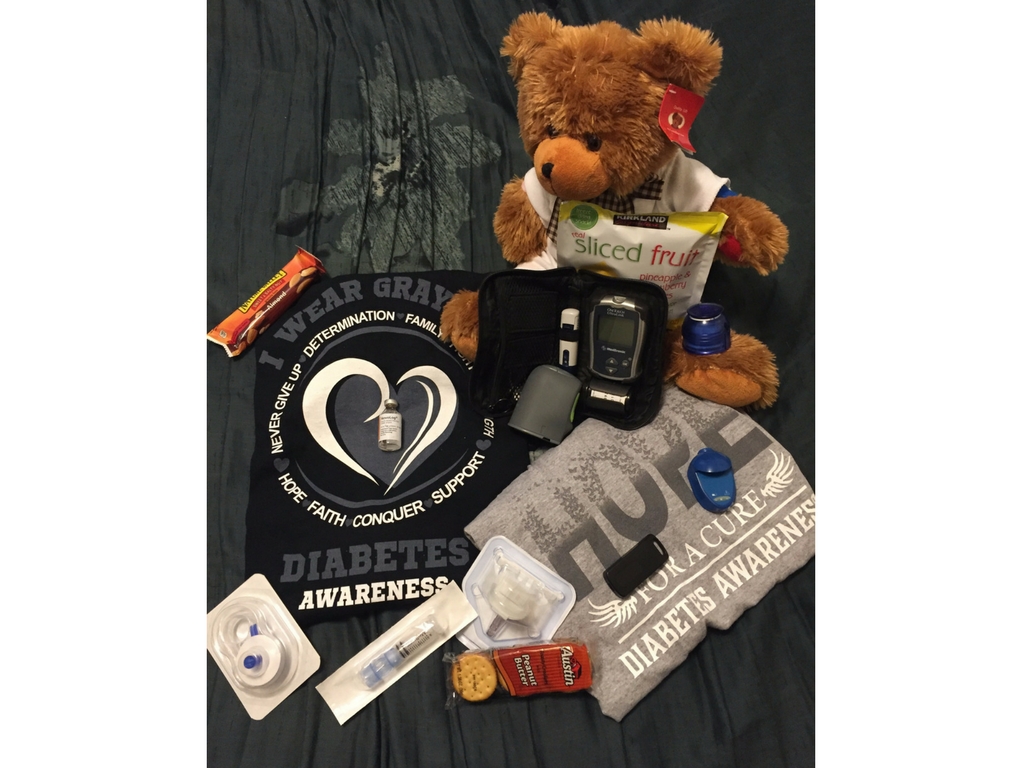
When you go to sleep at night you generally expect to wake up in the morning. When you have a chronic illness like Type 1 Diabetes, you try everything you can to make sure you will wake up the next morning.
You do everything right. But sometimes it’s not enough.
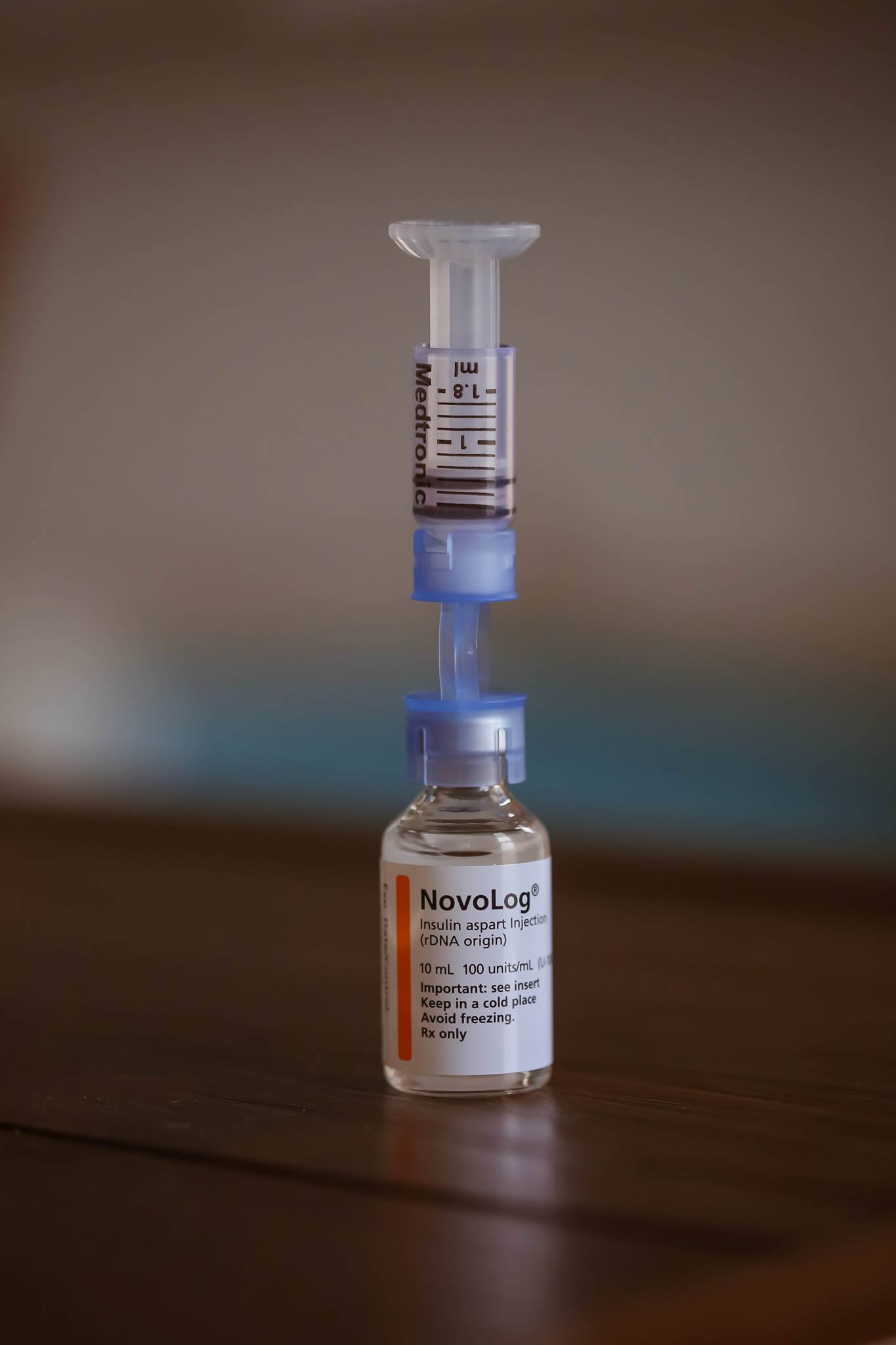
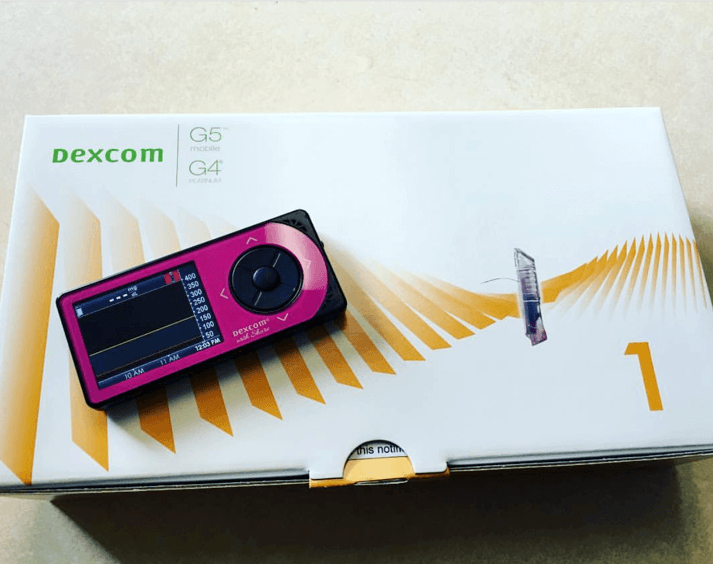
I am thankful to have technology that helps me stay alive, but I understand that technology is not perfect and sometimes things can still go wrong. Two weeks ago I went to bed like any other night, but woke up early the next morning with an intense feeling of desperation that I know all too well. My blood sugar was dropping. Fast.
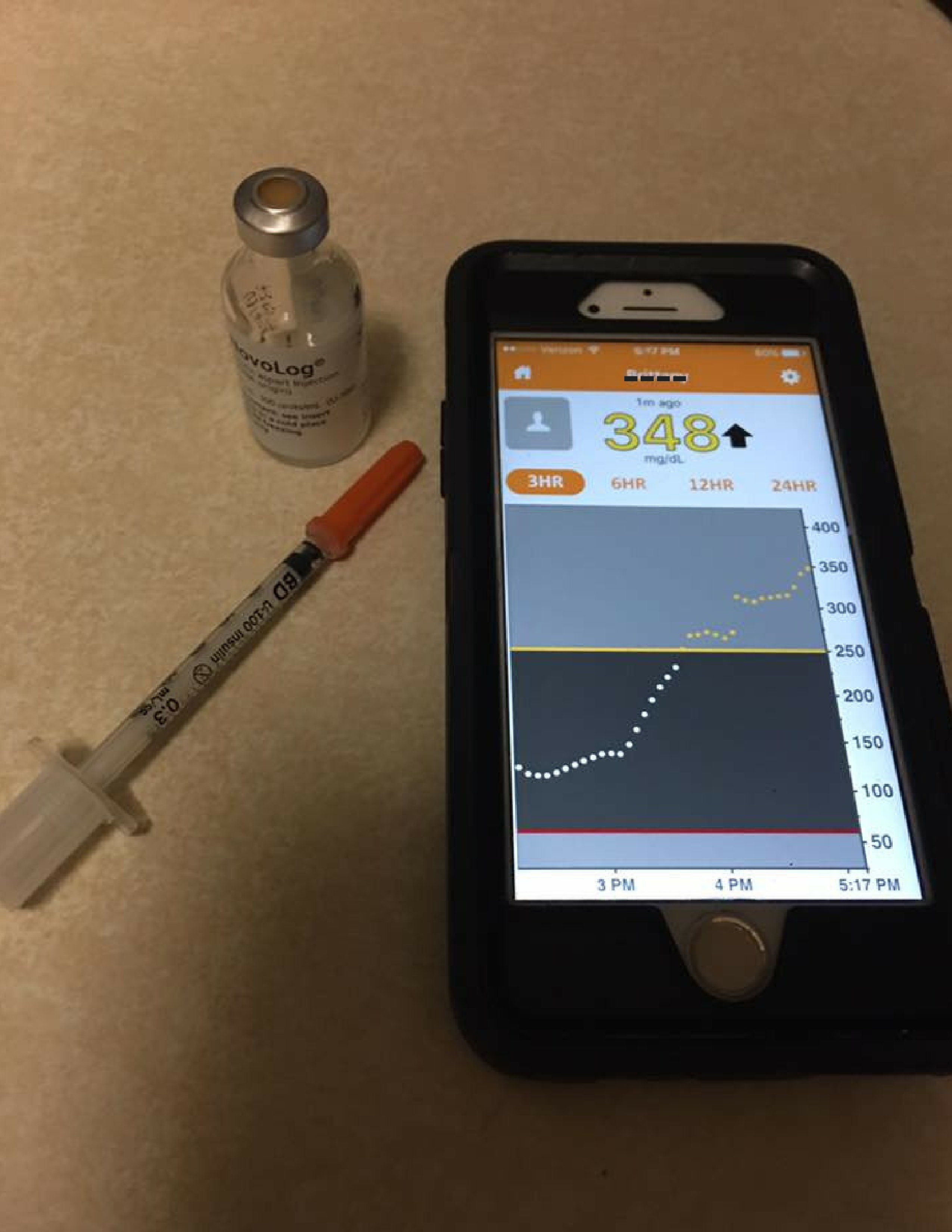
I looked at my phone to check my Dexcom app and it read 74 (which wouldn’t normally give me these symptoms). I knew the reading had to be wrong so I woke my husband up and told him to get me juice FAST. He did, along with my meter so I can see how much juice I might need. My meter read 49. And I can tell I was dropping to a lower number quickly, so I drank a 2nd juice.
The next 15 minutes felt like 15 hours. Heart racing, rapid breathing, physiology kicking in and telling you that you need more sugar now. But I know I must wait. It finally came back up and I woke up a couple of hours later at a completely normal blood sugar of 123.
Then I thought to myself, what if that 49 didn’t wake me up? What would’ve happened to me?
I clearly needed those 30 grams of carbs I drank since my blood sugar didn’t spike later. If I didn’t drink it, what would that morning have looked like for my family? Panic set in. The feelings of what if and the feelings of reality kicking in came over me. But why did my blood sugar drop so low?
Why do these things happen even if you live your life by a calculator and you dose your insulin as best you can and you try so hard? Because. Diabetes.
Diabetes has no rhyme or reason. Sometimes 2 + 2 does not equal 4. And sometimes you wake up before the sun because God decided that today is not that day. Today you will wake up. You will wake up before it’s too late.
Today, you will survive. And two weeks later, I’m still thankful.