This Is My Life Support, This Is Type 1 Diabetes
By: Katharine Orona
Instagram: @this_is_type_1_diabetes | Blog: thisistype1diabetes
10 years ago I was only a few weeks away from having my life turned upside down and changed forever. I was only weeks away from being diagnosed with an incurable disease, one I didn’t bring upon myself, and one I knew nothing about.
I was about to be diagnosed with Type 1 (LADA) Diabetes.
I had been the picture of health. Perfect blood work results at every checkup, thin, and young. I was 26 years old, about to get married, and recently promoted at work. It was then that I thought I had everything under control and everything seemed to be perfect.
I had all the classic symptoms but didn’t know what they meant: extreme thirst, frequent urination, and rapid unexplained weight loss (at 5 feet tall, I went from 106 lbs to 90 lbs in less than 3 months). My doctor knew right away it was diabetes when I went in with my symptoms. I went to the ER, was immediately admitted, and spent 5 days at the hospital.
After that it took me 5 years to come to terms with my disease.
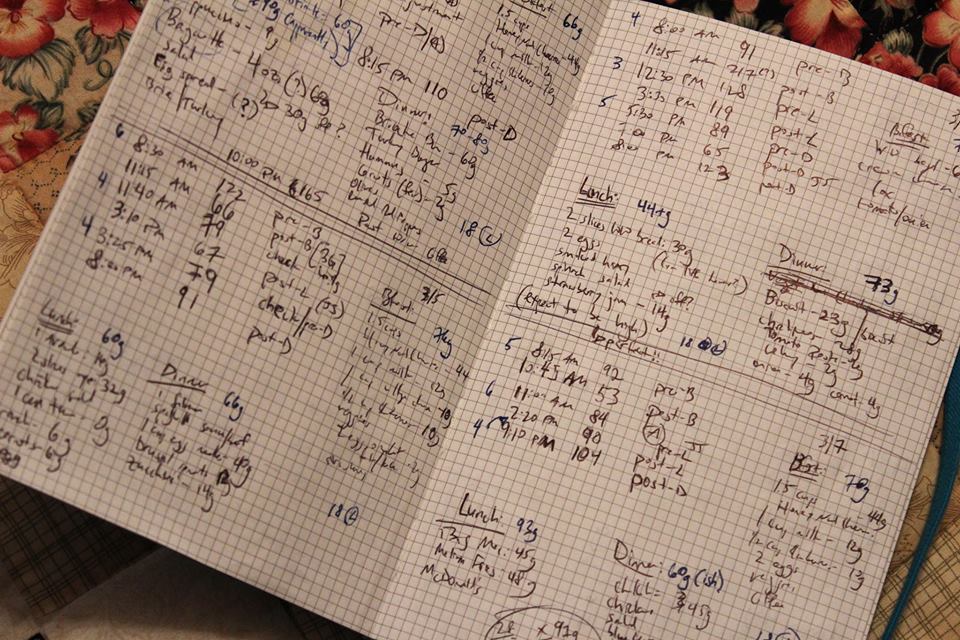
5 years to go through anger, denial, and grief over losing a life I had known for 26 years. 5 years to decide I was ready to start using a different form of treatment, an insulin pump.
I was so resistant to this technology. I saw it as life support, I saw it as a restriction, I saw it as something I would have to conceal and be ashamed about. When I was finally ready and took the plunge, I loved it from day one. To my surprise, it was freeing, not restricting.
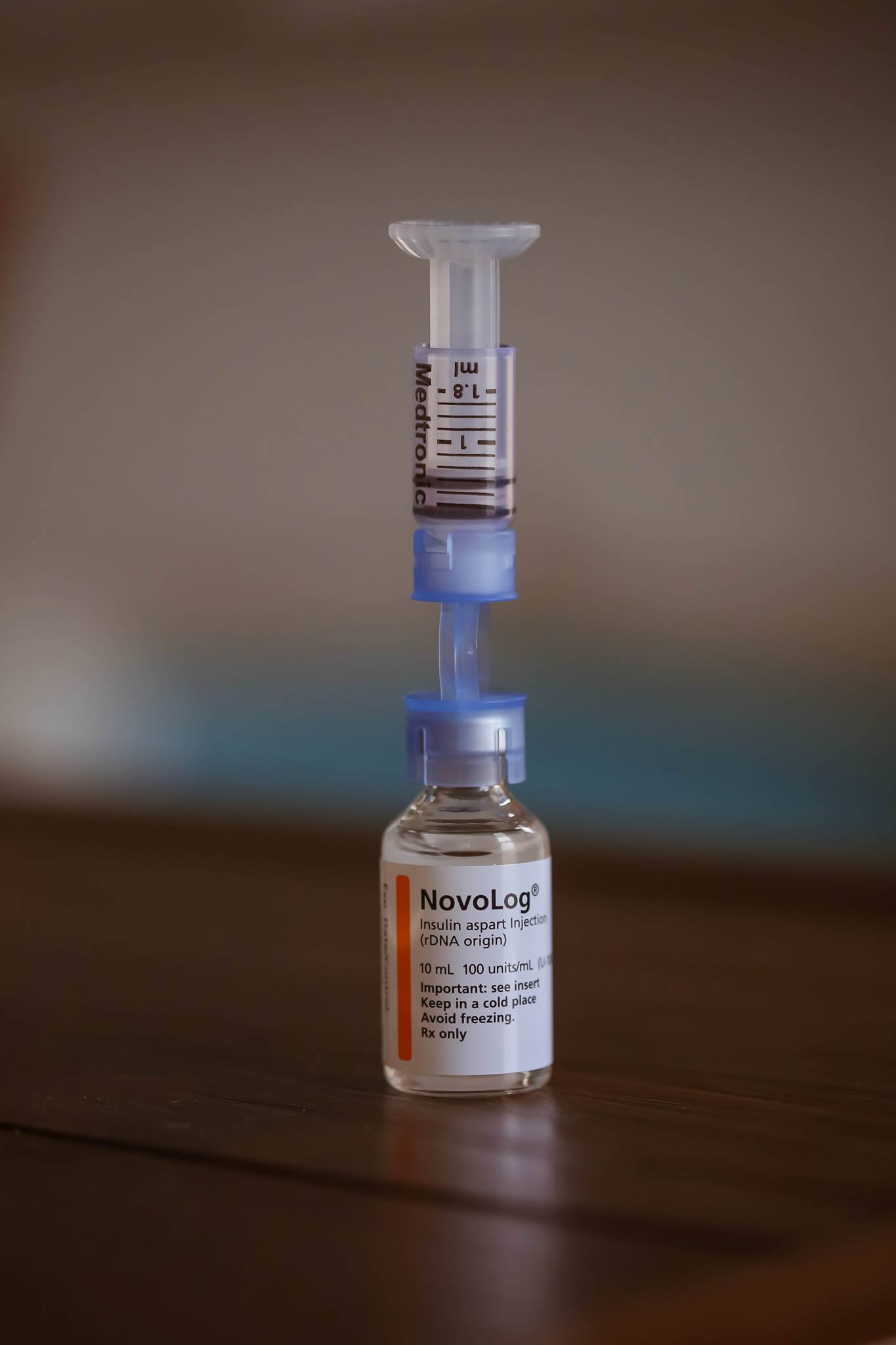
It is life support, but I am thankful for it.
However, I still felt the need to conceal it. I dreaded being asked questions about it or having people wonder why I was wearing a pager (90s folks you know what that is). I felt embarrassed that I needed something to live that other people did not. It took a long time to own it.
A few years later when I was pregnant with my son and my doctor suggested a continuous glucose monitor I went through the same feelings all over again. Another medical device? More things that will make it harder for me to pick an outfit that can conceal that too? But, I knew I had to do it so I did.
My son was worth every awkward stare and every question I faced.
These are tools that I use to make my life a tiny bit more normal. They keep me alive. When my son was born 5 weeks before his due date, and I later made the connection, I realized that he was born on the 6th anniversary of my diabetes diagnosis, at the same hospital I spent those first 5 days after diagnosis.
That fateful day in 2007 that I thought was the worst day of my life, turned out to be the best day of my life 6 years later.
Today I can finally say I not only wear my medical devices with pride, I rock them.
And no matter what method of treatment you choose, know that it’s keeping you alive and you are stronger because of it. Feel comfortable with whatever makes you different. Because it makes you YOU.
As Dr Seuss once said: “Today you are You, that is truer than true. There is no one alive who is Youer than You.”