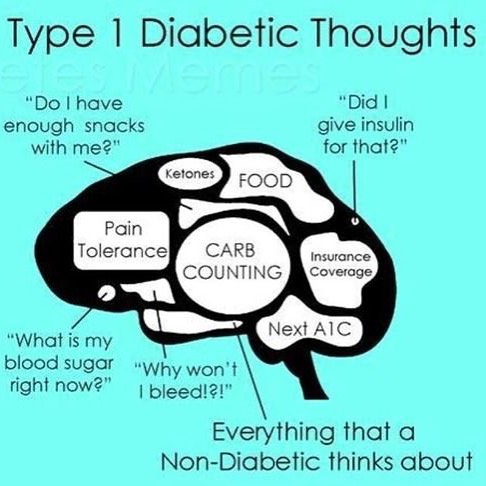
Having Type 1 Diabetes is challenging yet it becomes part of our everyday routine. To the outside world what a type 1 diabetic deals with may seem unimaginable, but to those in the diabetes community we totally get it and can find humor in our everyday lives.
The Best of ‘You Know You’re a Type 1 Diabetic When’
1. You accidentally cut yourself and wonder if you can get enough blood to test your sugar.
2. Explaining to worried teenagers in the public restroom….”I am taking an insulin shot because I am a type 1 diabetic, I’m not a junkie”.
3. When you look at food and see numbers.
4. When your finger tips look like they need blackhead removal.
5. You have a drawer of candy for emergencies.

7. When you’re scooping out the very last scoop of ice cream from the container and haven’t had time to bolus for it yet and your husband comes into the kitchen and wants some and you look at him innocently and say “oh, I’m sorry I just bolused for that”.
8. When you wake up with a test strip stuck to your face.
9. When someone tells you that cinnamon can fix all your problems.
10. You are up all night correcting or being forced fed when all you want to do is sleep.
11. When someone thinks you’re drunk but you are really just low.
12. When the butter compartment in your fridge is no longer used for butter.

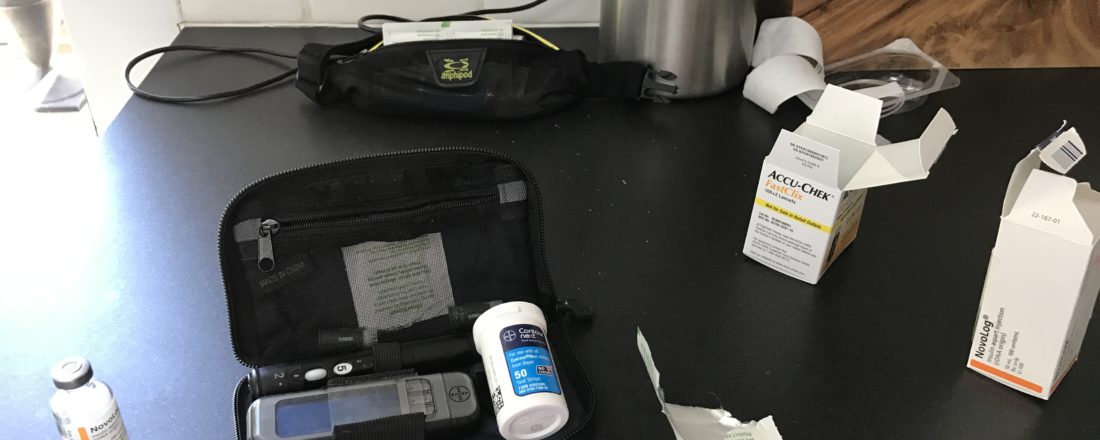
13. When your outfit revolves around if it can hold your pump up or not.
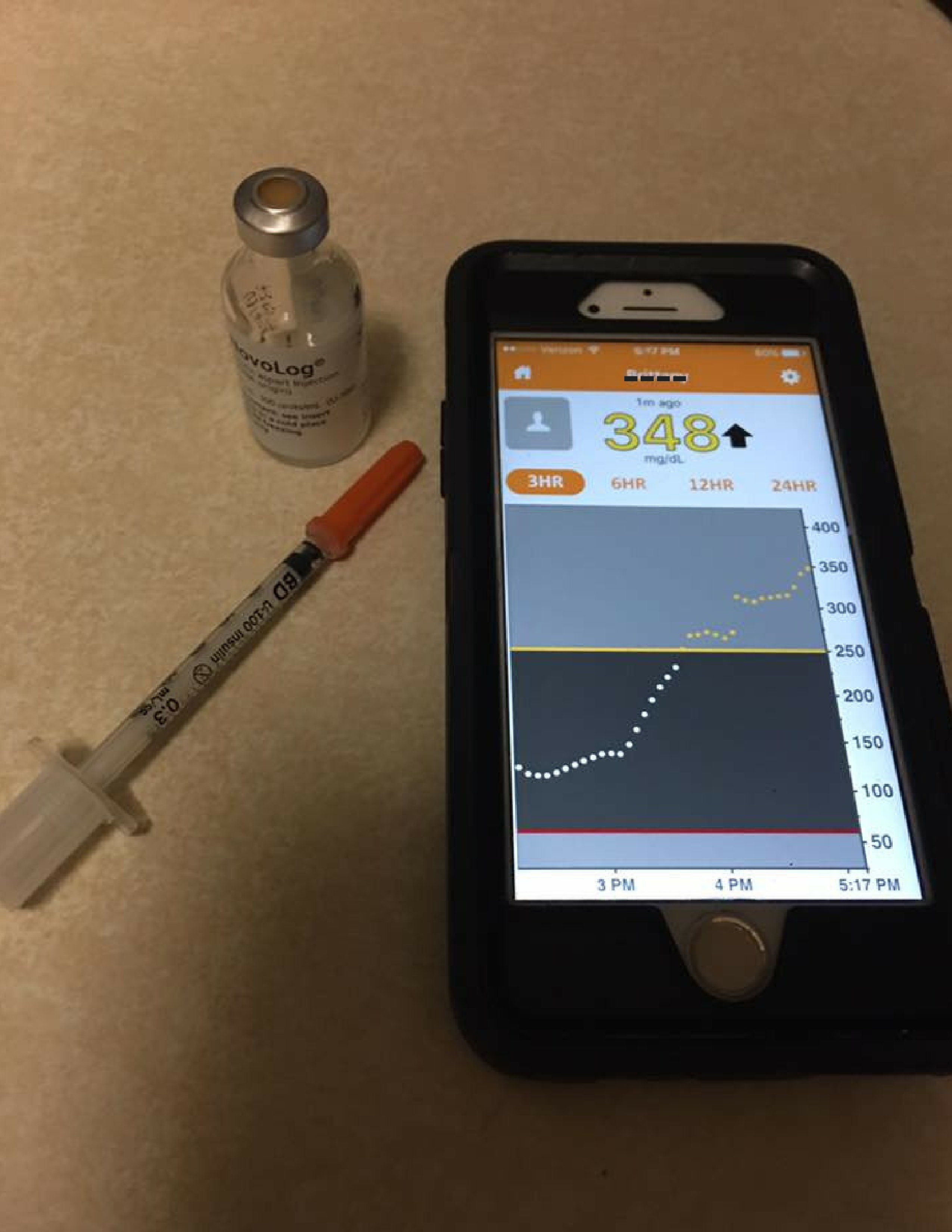
14. One day your fasting can be a perfect 77 and the next day it’s 343.
15. When your handbag is the size of a suitcase to carry all your diabetes stuff around plus your ‘normal’ stuff.
16. When you have to pee like a race horse in a Kentucky derby.
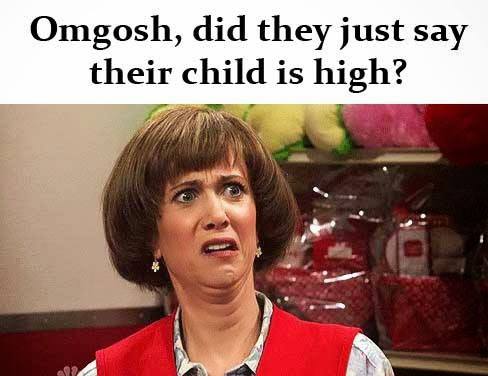
17. When your mom, in front of everyone says, “baby, you are high!”
18. When you get up during the night going low, invade the goodies cupboard and turn into a complete savage then wake in the morning like you’ve been out drinking too much.
19. When you wanna punch someone in the face but turns out you just need a snack.
20. You have headaches and you think your sugar is really high but you realize its just a normal headache.

22. You’re cramming gummy bears in your mouth while prepping dinner.
23. When you automatically know what your pump is telling you without looking because of the sound it’s making.
24. When you chew open the corner of a juice box for a 3 am crash after losing the straw.
25. Your wallet is empty.
26. When your zombie apocalypse plan involves looting a pharmacy, a cooler, and travel to a colder climate.
27. You are excited beyond words to see a sugar-free line of drinks from Monster Energy.
29. When you tell people you have to shoot up to avoid getting high!
30. You’re excited that you’re blood sugar is low because you really have been wanting to eat. [Fill in the blank with your favorite cheat food].
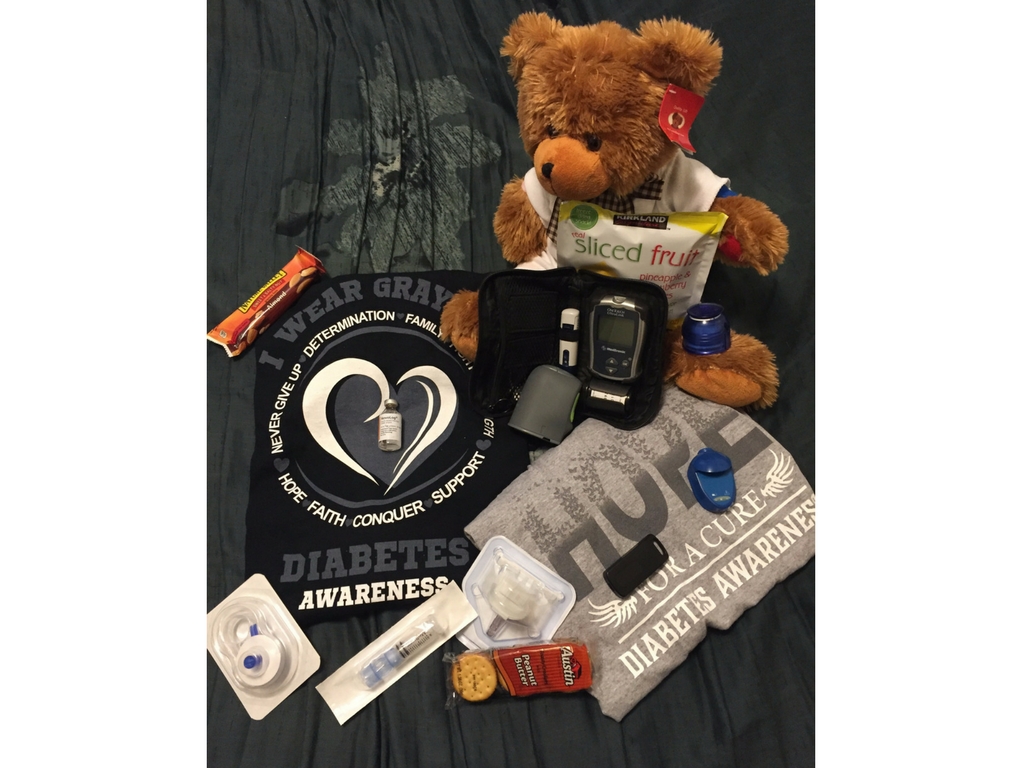
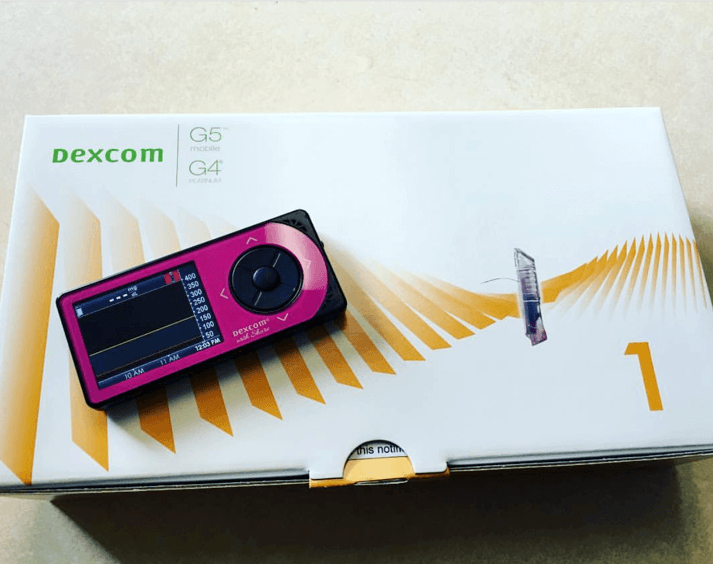
31. When you get excited from receiving your medical supply shipment in the mail.
32. You pull a pump out of your bra at the dinner table.
33. When you are skilled at giving yourself a shot in a moving vehicle.
34. You buy all the holiday candy for your low “stash”.
35. When you’re the only person in the gym with candy and juice boxes.
36. When someone asks you for your phone number but you give them your blood sugar number.
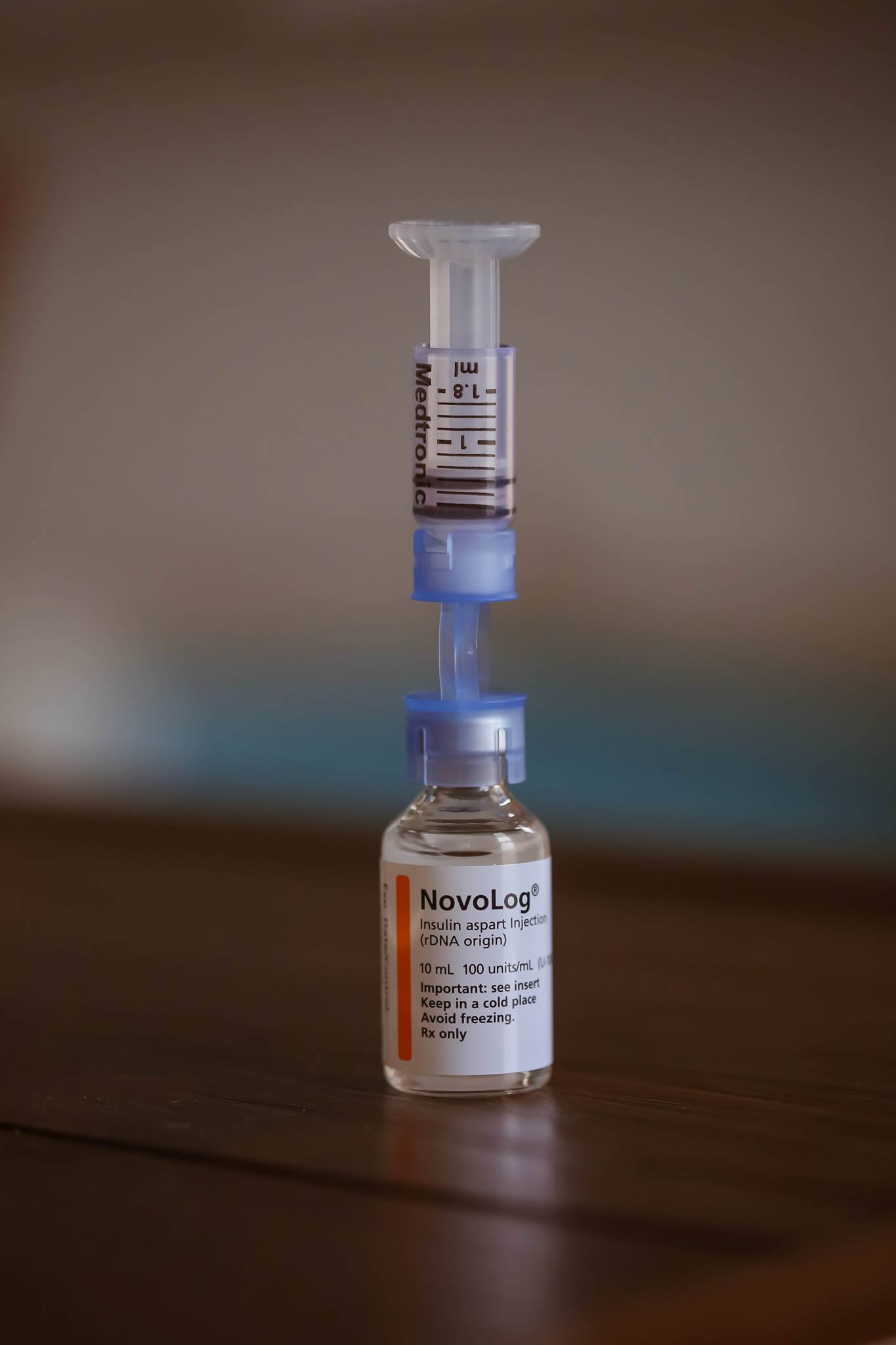
38. When insulin is LIFE.
39. When you blame being in a bad mood on your sugar being high.
40. Your worst and best subject is math.
41. When you have to eat before you go out to eat.
—
**Comment with your favorite ‘You Know You’re a Type 1 Diabetic When’